Range of Motion: The Gateway Into the Body’s Mechanics
Diagnosing injuries, pain, or impairments can often be a challenging puzzle. A patient’s range of motion offers a solid foundation from which to begin any diagnosis and treatment plan. JTECH Medical reached out to experts in a variety of fields to find out when, how, and why they use inclinometry in their practices.
A recurring sentiment among clinicians across multiple disciplines and with a variety of goals is that range of motion is the gateway into the body’s mechanics.
“Range of motion is the backbone of what anyone in physical medicine is doing,” says Alireza Bagherian, DC. “Motion is where it all starts, and it plays into each of the other aspects of the physical evaluation. It is the foundation where the functional assessment begins.”
Jenny Adams, a senior research associate at Baylor Hamilton Heart and Vascular Hospital in Dallas, Texas, aims to help patients “return to life” after a heart event. In order to help determine the best program for reaching this goal, Adams’ clinic incorporates digital range of motion analysis into their program.
“We want to do pre- and post-testing for muscular strength, cardio, and flexibility too (for outcomes reporting),” says Adams. “Traditionally, the ‘sit and reach’ test has been offered as a way to test for flexibility in cardiac rehab programs. This test is usually performed on the floor and is (to us) really an indication of hamstring tightness and not overall flexibility. Furthermore, many patients have no desire to sit on the floor to do this test. Having access to inclinometry enables us to test any body part for flexibility, take note of patients who have problems, offer activities to perform over the course of rehab and then re-test and see if there is improvement in the patient’s ability to perform their activities of daily living following a heart event.”
As the terminology in Adams’ approach suggests, range of motion is a key component to everyday activities. If a patient is experiencing difficulties with their range of motion, it can impact other aspects of their lives and treatment plans.
“It is very difficult to increase strength without first achieving a healthy range of motion,” says Don Counihan, DC. “A patient may avoid certain movements because of pain or out of fear of further injury. If you begin with an accurate overview of their mobility and a treatment plan that addresses any deficits, then you can more naturally progress towards strength improvements.”
Indeed, with range of motion acting as the gateway to any analysis, the path towards a correct diagnosis and a viable treatment plan becomes much clearer.
“If you collect dual inclinometry data on a patient, you have tangible evidence that the patient has a deficit in their ability,” says Dr. Bagherian. “It also gives you objective data to measure against, so when the patient comes in for a follow-up exam, you can see whether or not the range of motion has improved. If it hasn’t improved, you can begin to explore other options. Providing care feels good, so it’s important to have this data to know when to stop, or adjust the plan to new expectations. A patient may never reach 100% range of motion, and recognizing these plateaus is a crucial component of a strong rehab program.”
But the benefits of range of motion information can be limited if it is not objective. Computerized inclinometers offer a level of reproducibility and objectivity that simply cannot be achieved with standard handheld devices.
“Clinician’s observations are not repeatable or defensible,” says Jonathan Reynolds, PT, PhD. “In some situations, a patient’s improvement may be subtle, particularly with the spine, and may not be observably different. I have found that in many cases, a non-observable difference can be detected with a fine measurement, such as dual inclinometry.”
The objective data can prove beneficial to the patient as well, offering a visual marker of improvement when the results may not be dramatic enough to notice a change.
“Exact measurements are critical because patients can see the numbers, make goals for improvement and then see if they improved,” says Adams. “Having a ‘shoulder issue that we work on’ is something non-tangible, but having numbers and improving those numbers over the course of rehab is a powerful motivational tool and helps us know if we are doing a good job with our activity prescription as well.”
“Of course a protractor would still work,” says Dr. Bagherian, “but why would you use one? Computerized inclinometers provide objective measurements, which can be used to automatically calculate validity, reliability, and reproducibility using the coefficient of variation. The software allows you to do in 5 minutes what would take you 15 or more if you did it manually—not to mention, the increase in possibility of error.”
Computerized inclinometers also offer the advantage of using two inclinometers that share data. Dual inclinometry allows the clinician to isolate the specific motion and avoid erroneous measurements.
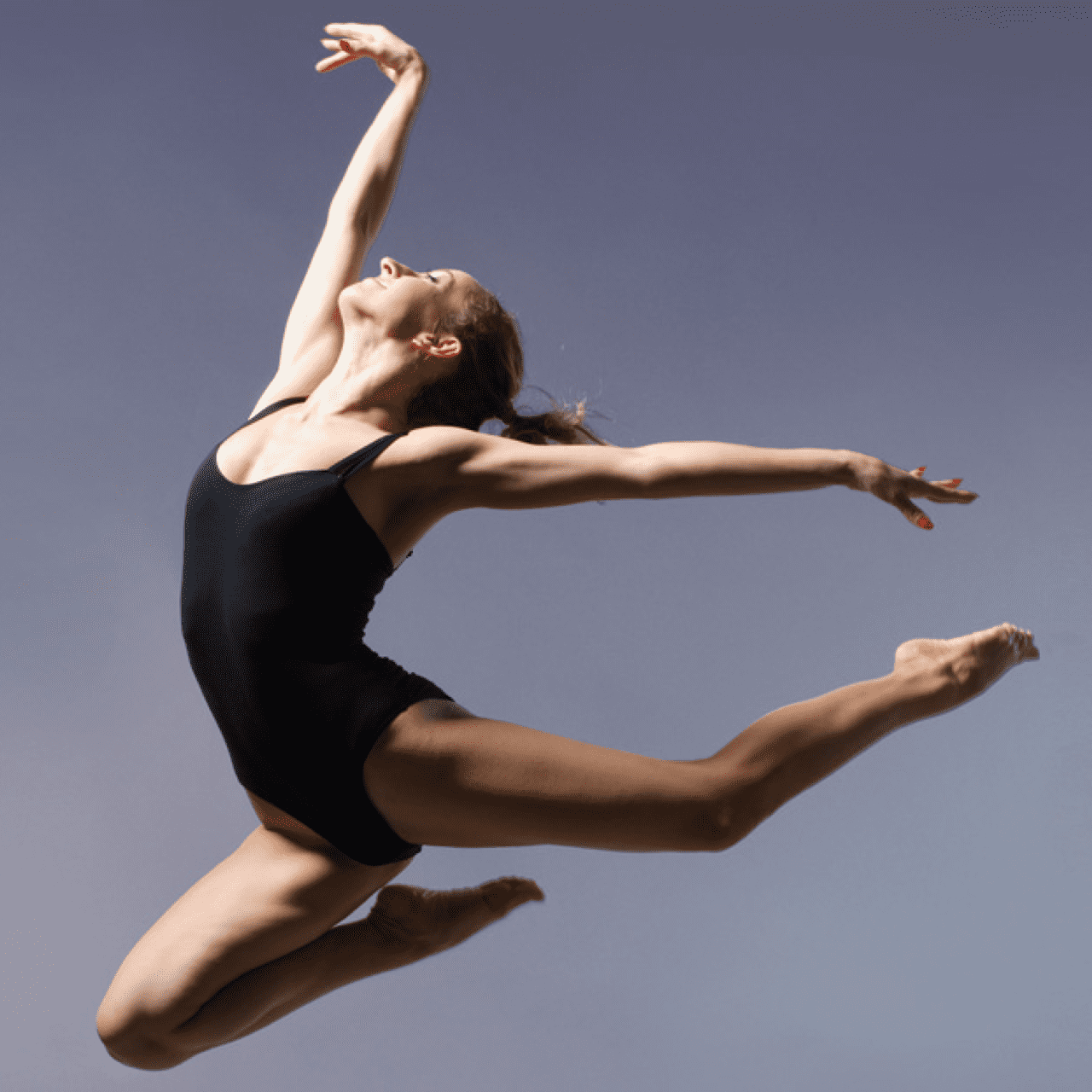
“Dual inclinometry is really important as it reduces the measurement error by eliminating movement of the proximal segment of the joint,” says Dr. Reynolds. “One of the biggest criticisms of joint range of motion measurement is evaluator error. If one can reduce this error and demonstrate a level of proficiency in exam performance, this makes defensibility of results very important. Dancers with back pain measurement are a great example. They are so flexible in their hamstrings that they appear to have good spine range of motion, and are sometimes dismissed by clinicians having no limitations. In fact, they have significant spine range limitations that are hidden by hamstring flexibility. This is a classic reason to use dual inclinometers.”
Regardless of the injury or treatment goal, range of motion is an integral component to physical evaluations and rehabilitation programs. Computerized inclinometers provide a foundation from which to build a diagnosis and map out a treatment plan.
“Records are only as good as the story you can tell from them,” says Dr. Counihan, “and a range of motion evaluation sets the stage for the rest of the story to play out. It may not be fancy, and it’s not going to impress, but it is the marker for what is or is not moving properly, and that’s what will help you guide the patient back to normalcy.”
